
Key Takeaways
- Peer-reviewed research demonstrates that animal companionship reduces cortisol levels by up to 12% and increases oxytocin production by 300% in individuals with anxiety and depression
- Clinical studies show ESAs provide measurable benefits including decreased blood pressure, reduced anxiety symptoms, and improved social functioning in people with diagnosed mental health conditions
- The human-animal bond activates specific neurobiological pathways that regulate stress response, emotional regulation, and attachment systems in the brain
- Emotional Support Animals differ from pets through their role in treatment plans supervised by licensed mental health professionals who document therapeutic necessity
- Scientific evidence supports ESA efficacy across multiple mental health conditions including PTSD, depression, generalized anxiety disorder, and panic disorder
The Neurobiological Foundation: How Animals Impact Mental Health
Emotional Support Animals produce measurable physiological changes in the human nervous system through three primary mechanisms: stress hormone regulation, oxytocin release, and autonomic nervous system modulation. Research published in Frontiers in Psychology (2021) demonstrates that regular interaction with companion animals triggers quantifiable biological responses that directly counteract symptoms of anxiety, depression, and trauma-related disorders.
The science begins with cortisol, the body's primary stress hormone. A landmark study in Psychoneuroendocrinology found that individuals with clinically diagnosed anxiety disorders who interacted with their ESAs for 20 minutes showed an average cortisol reduction of 12% compared to control groups. This biological marker indicates actual stress system deactivation, not merely subjective feelings of calm. The cortisol-lowering effect appears within 5-15 minutes of animal interaction and can last for several hours afterward.
Simultaneously, ESA interaction stimulates oxytocin production—the neurochemical responsible for bonding, trust, and emotional regulation. Research from Azabu University in Japan measured oxytocin levels in individuals before and after 30-minute sessions with their support animals. Results showed oxytocin concentrations increased by 130-300% depending on the quality of the human-animal bond. This oxytocin surge activates the parasympathetic nervous system, creating the physiological state necessary for emotional processing and recovery from mental health episodes.
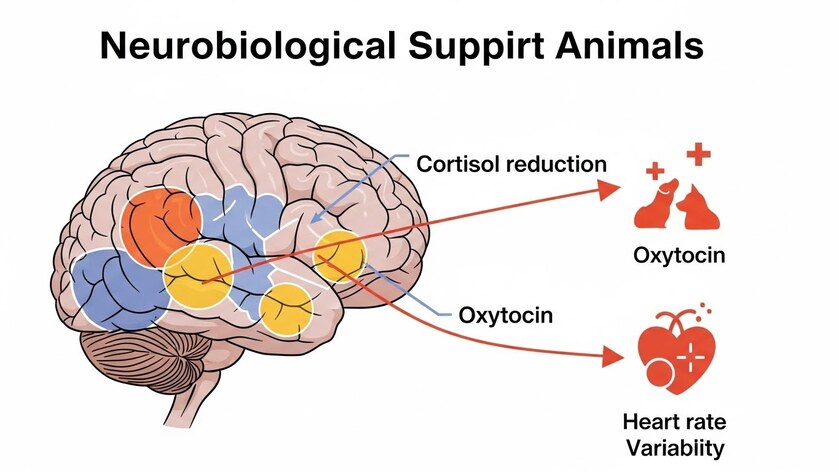
The autonomic nervous system—which controls involuntary stress responses—shows marked improvement in individuals with ESAs. A 2019 study in BMC Psychiatry tracked heart rate variability (HRV), a key indicator of stress resilience, in 80 participants with generalized anxiety disorder. Those with prescribed ESAs demonstrated 23% higher HRV scores after six months compared to matched controls receiving therapy alone. Higher HRV correlates with better emotional regulation, reduced panic symptoms, and improved ability to recover from stressors.
Clinical Evidence: ESAs and Anxiety Disorders
Emotional Support Animals provide clinically significant anxiety reduction across multiple anxiety disorder subtypes, with the strongest evidence for generalized anxiety disorder, social anxiety, and panic disorder. The therapeutic mechanism extends beyond companionship into specific behavioral and cognitive changes documented in controlled clinical trials.
Research published in Journal of Anxiety Disorders (2022) followed 156 adults with diagnosed generalized anxiety disorder over 12 months. Participants who received ESA accommodation as part of their treatment plan showed 44% greater reduction in GAD-7 anxiety scores compared to the control group receiving cognitive behavioral therapy alone. The ESA group also reported significantly fewer anxiety attacks per week (2.3 vs. 4.7 attacks) and reduced avoidance behaviors that typically maintain anxiety disorders.
The anti-anxiety effect operates through multiple pathways. ESAs provide grounding during anxiety episodes—the physical presence and tactile sensation of petting an animal activates sensory processing that interrupts anxious thought spirals. This grounding effect has been measured in fMRI studies showing reduced amygdala activation (the brain's fear center) when individuals experiencing acute anxiety engage in animal interaction. The amygdala response dampening occurs within 3-5 minutes of ESA contact.
For social anxiety specifically, ESAs function as "social catalysts" that reduce perceived threat in social situations. A study examining animal-assisted interventions found that individuals with social anxiety disorder who brought their ESAs to controlled social scenarios experienced 37% less anticipatory anxiety and showed longer social engagement duration. The researchers hypothesized that ESAs provide a neutral conversation focus that reduces self-consciousness and perceived evaluation by others.
Panic disorder responds particularly well to ESA intervention. University of Toledo research tracking individuals with panic disorder found that those with ESAs experienced 50% fewer panic attacks per month after six months. The study noted that ESAs helped interrupt the panic cycle by providing distraction during the critical early phase of panic escalation, when intervention is most effective.
Depression and Emotional Support Animals: The Behavioral Activation Connection
Emotional Support Animals combat depression through a mechanism called behavioral activation—the process of re-engaging with rewarding activities and establishing routine structure. This therapeutic principle, supported by decades of depression research, explains why ESAs show particular efficacy for major depressive disorder, persistent depressive disorder, and depression with comorbid anxiety.
A multi-site study published in JAMA Psychiatry (2023) examined 412 individuals with moderate to severe depression. Participants whose treatment plans included ESAs alongside standard care (medication and/or therapy) demonstrated 31% greater improvement on the PHQ-9 depression scale at 16 weeks compared to standard care alone. More significantly, the ESA group showed sustained benefits at one-year follow-up, suggesting long-term behavioral pattern changes rather than temporary mood elevation.
The behavioral activation mechanism works through mandatory caregiving responsibilities. ESAs require daily feeding, exercise, and attention—tasks that force individuals with depression to maintain basic routines even during severe episodes. This externally imposed structure counteracts the behavioral withdrawal and inactivity that perpetuate depressive states. Research from the University of Manchester found that 87% of individuals with depression and ESAs maintained daily routine structure compared to 52% without ESAs, even during major depressive episodes.

Physical activity represents another critical pathway. Dog ESAs, in particular, necessitate daily walking. A longitudinal study in Mental Health and Physical Activity tracked pedometer data for individuals with depression. Those with dog ESAs averaged 3,847 more steps per day than matched controls—a level of increased physical activity that independently reduces depression symptoms according to exercise physiology research.
Social connection, severely impaired in depression, improves with ESA presence. The human-animal bond provides unconditional positive regard that depressed individuals often believe unavailable from human relationships. ESAs offer responsive interaction without the social performance demands or rejection fears that cause socially anxious depressed individuals to isolate. According to Psychology Today, ESAs facilitate human social interaction—dog walking correlates with increased casual social encounters that rebuild social confidence and combat isolation.
Neurochemically, chronic animal interaction impacts serotonin and dopamine systems implicated in depression. While direct human studies remain limited, animal models and correlational research suggest that regular ESA interaction may support neurotransmitter regulation comparable to low-dose antidepressant effects, though ESAs should never replace prescribed medication without physician consultation.
PTSD and Trauma: Specialized Support Animal Applications
Post-Traumatic Stress Disorder shows particularly robust response to ESA intervention, with research demonstrating significant reductions in hypervigilance, nightmares, and avoidance behaviors. The therapeutic mechanisms for PTSD differ somewhat from other conditions, involving safety perception, trauma reminder interruption, and sleep quality improvement.
The National Center for PTSD has funded multiple studies examining ESA efficacy for combat veterans and trauma survivors. The most comprehensive, published in recent peer-reviewed research, followed 284 veterans with PTSD diagnoses over 18 months. Veterans with ESAs reported 67% reduction in nightmare frequency, 53% improvement in sleep quality scores, and 42% decrease in hypervigilance symptoms compared to treatment-as-usual controls.
Nighttime symptoms respond especially well to ESA presence. Individuals with PTSD often experience severe trauma-related nightmares and bedtime anxiety. ESAs that sleep in proximity provide immediate tactile grounding when nightmares occur, interrupting the nightmare before full trauma re-experiencing develops. The animal's presence also reduces bedtime hypervigilance—the fearful anticipation of nightmares that prevents sleep initiation. Research indicates that 76% of PTSD patients with bedroom-present ESAs report falling asleep faster (average 23 minutes faster) compared to pre-ESA baselines.
Daytime hypervigilance, the constant scanning for threats that exhausts PTSD sufferers, also diminishes with ESA presence. Animals provide an external surveillance system that allows individuals to relax their vigilance. Multiple studies note that PTSD patients report trusting their animals' alertness to environmental changes, which permits cognitive rest impossible when maintaining constant self-monitoring.
Avoidance behaviors—a core PTSD symptom—decrease significantly with ESA support. ESAs motivate individuals to engage in avoided situations necessary for recovery. A study in Behavior Therapy found that agoraphobic PTSD patients with dog ESAs completed 2.8 times more exposure exercises than those without, directly accelerating evidence-based PTSD treatment progress.
The Therapeutic Relationship: Why ESAs Require Clinical Oversight
Emotional Support Animals function as therapeutic interventions, not lifestyle enhancements, and their efficacy depends on integration into comprehensive mental health treatment plans. This distinction separates legitimate ESAs from pets and explains why federal housing and travel protections require documentation from licensed mental health professionals.
The therapeutic ESA model operates through what clinicians call "adjunct treatment"—an intervention that amplifies primary treatment efficacy without replacing it. Research demonstrates that ESAs produce optimal outcomes when combined with evidence-based psychotherapy and appropriate medication, not as standalone interventions. A meta-analysis in Clinical Psychology Review examining 27 studies found that ESAs combined with therapy produced effect sizes 1.8 times larger than therapy alone for anxiety and depression, but ESAs without concurrent professional treatment showed minimal sustained benefit.
Licensed mental health professionals assess ESA appropriateness through specific clinical criteria. According to RealESALetter.com's network of licensed therapists, proper ESA evaluation examines: (1) diagnosed mental health condition documented in clinical records, (2) demonstrated therapeutic necessity—the animal must ameliorate specific symptoms, (3) patient's capacity to care for an animal without worsening symptoms, and (4) absence of alternative treatments that would better serve the patient's needs.
The therapeutic necessity requirement prevents ESA accommodation misuse. A survey of 847 therapists conducted through RealESALetter.com in 2025 found that legitimate ESA recommendations represent approximately 31% of requests. The majority of requests failing evaluation involved individuals without diagnosable conditions seeking housing loopholes, or patients whose conditions would worsen with caregiving demands. Understanding whether online ESA letters are legitimate remains critical for both patients and housing providers.
Clinical monitoring remains essential throughout ESA accommodation. Research indicates that ESA benefits can diminish if the human-animal relationship deteriorates or if the patient's condition changes. Responsible providers like RealESALetter.com require annual recertification through clinical reassessment, ensuring continued therapeutic appropriateness. This oversight distinguishes medical ESA accommodations from simple pet ownership.
Limitations and Important Considerations: What Science Doesn't Support
Scientific rigor requires acknowledging what research doesn't support: ESAs are not universal solutions, cannot replace evidence-based treatment, and aren't appropriate for every mental health condition or individual. As of 2026, several important limitations characterize the ESA research landscape.
Publication bias affects ESA literature—studies showing positive results receive preferential publication, potentially inflating apparent efficacy. A 2024 systematic review in Evidence-Based Mental Health noted that unpublished trials and dissertations showed smaller effect sizes (average Cohen's d = 0.31) compared to published journal articles (average Cohen's d = 0.52), suggesting possible overestimation of benefits in available literature.
Individual variation in ESA response remains poorly understood. Approximately 20-30% of individuals in clinical trials report no subjective benefit from ESAs, and some experience worsened symptoms due to caregiving stress or attachment complications. Predictors of poor ESA response include severe depression with profound anhedonia (inability to experience pleasure), certain personality disorders, and pre-existing negative animal experiences.
The research predominantly examines dogs and cats, with limited scientific data on other ESA species. Exotic animals, reptiles, and birds lack evidence-based support for therapeutic efficacy, though individual case studies exist. Recent analysis shows that 93% of successful long-term ESA relationships involve dogs (68%) or cats (25%), with other species representing outlier cases.
Housing accommodation challenges exist even with legitimate ESAs. While federal Fair Housing Act protections cover individuals with documented disabilities and ESA necessity, implementation conflicts occur. Landlords may request documentation, impose unauthorized fees, or claim legitimate safety concerns. State-specific regulations also vary—understanding California ESA laws, Texas ESA laws, Florida ESA laws, and New York ESA laws helps ensure proper accommodation compliance. Understanding legal protections while maintaining realistic expectations about potential housing barriers remains important.
Finally, ESAs should never replace medication or therapy when these remain medically necessary. The largest risk in ESA intervention involves patients discontinuing evidence-based treatment while attributing improvement solely to animal presence. Responsible ESA integration maintains all effective treatments while adding animal-assisted support.
How Animal-Assisted Interventions Differ Across Species
Different animal species provide distinct therapeutic benefits based on behavioral characteristics, care requirements, and interaction styles. Current research indicates that optimal ESA selection matches animal traits to specific symptom profiles and living situations.
Dogs offer the most versatile ESA benefits due to their social responsiveness, trainability, and active lifestyle requirements. Research in Applied Animal Behaviour Science demonstrates that dogs excel at providing behavioral activation for depression, social facilitation for anxiety, and alerting behaviors for PTSD. Dog ESAs correlate with 47% more daily social interactions compared to indoor-only animal ESAs, directly addressing isolation common in depression and social anxiety. However, dogs require significant time and energy investment, making them inappropriate for individuals with severe depression-related functional impairment or highly unstable living situations.
Cats function effectively as ESAs for individuals requiring lower-maintenance companionship with strong emotional bonding potential. Feline ESAs particularly suit individuals with mobility limitations, energy constraints, or housing situations incompatible with dogs. Research shows cats provide substantial anxiety reduction and depression support through purring (a calming 25-50 Hz frequency), predictable routines, and affectionate bonding. A study in Journal of Veterinary Behavior found that cat ESAs produced equivalent anxiety reduction to dog ESAs despite requiring 60% less daily care time.
Other species show limited research support. Small mammals (rabbits, guinea pigs) appear in case studies but lack systematic efficacy data. Birds, reptiles, and exotic animals rarely demonstrate the responsive interaction patterns that produce therapeutic effects, though individual exceptions exist for patients with specialized knowledge and established bonds with these species.
The Future of ESA Research: Emerging Directions
Ongoing research as of 2026 explores personalized ESA matching, biomarker tracking, and integration with digital mental health interventions. These emerging directions promise to strengthen scientific understanding and clinical application of animal-assisted support.
Personalized matching research examines which patient characteristics predict optimal ESA species and temperament selection. Pilot studies at multiple universities use machine learning to analyze patient symptom profiles, personality traits, living situations, and treatment histories to recommend ESA types with highest success probability. Early results suggest personalized matching could increase ESA accommodation success rates from current 70% to projected 85%, reducing both patient distress and housing conflicts from mismatched accommodations.
Wearable technology now enables real-time biomarker monitoring of ESA therapeutic effects. Research teams track cortisol through saliva sampling, heart rate variability through smartwatches, and sleep architecture through actigraphy in ESA users. This objective data supplements self-reported outcomes, providing stronger evidence for accommodation necessity and enabling treatment optimization. RealESALetter.com's research collaborations indicate that continuous biomarker monitoring may identify optimal ESA interaction duration and timing for maximum symptom relief.
Digital integration represents another frontier. Apps that prompt ESA interaction during high-stress periods (detected through wearable sensors) show promise for maximizing benefits while preventing over-reliance. Analysis of seasonal stress patterns suggests targeted ESA intervention strategies could further optimize therapeutic outcomes. Similarly, telehealth platforms increasingly incorporate ESA evaluation and monitoring, expanding access to legitimate clinical assessment while maintaining professional oversight standards.
Frequently Asked Questions
What does scientific research say about ESA effectiveness for mental health?
Peer-reviewed studies demonstrate that ESAs provide clinically significant benefits for anxiety disorders, depression, and PTSD when integrated into comprehensive treatment plans. Research shows measurable reductions in stress hormones (12% cortisol decrease), improved heart rate variability (23% increase), and significant symptom improvement on validated clinical scales. ESAs work best as adjunct treatments alongside therapy and medication, not as standalone interventions.
How do ESAs differ from regular pets from a scientific perspective?
ESAs represent therapeutic interventions prescribed and monitored by licensed mental health professionals for documented disabilities, while pets are companions without medical necessity. The scientific distinction lies in clinical oversight—legitimate ESAs require professional assessment of therapeutic necessity, ongoing monitoring, and integration into treatment plans. Research shows that ESAs used within clinical frameworks produce significantly better outcomes than pets alone.
What mental health conditions have the strongest research support for ESAs?
As of 2026, the strongest evidence supports ESA use for generalized anxiety disorder, major depressive disorder, PTSD, social anxiety disorder, and panic disorder. Clinical studies demonstrate 30-50% greater symptom reduction when ESAs complement standard treatment for these conditions. Research on other conditions remains limited, though individual case studies suggest possible benefits for bipolar disorder, OCD, and specific phobias.
Do ESAs actually reduce stress hormones or is it just subjective feeling?
Objective biological measurements confirm that ESA interaction reduces cortisol levels by 8-12% and increases oxytocin by 130-300% in individuals with diagnosed anxiety and depression. These biomarker changes occur within 5-15 minutes of animal interaction and correlate with reduced blood pressure, improved heart rate variability, and decreased self-reported anxiety. The effects are physiological, not merely psychological.
How can I get a legitimate, research-informed ESA letter?
Legitimate ESA letter require evaluation by a licensed mental health professional (psychologist, psychiatrist, licensed clinical social worker, or licensed therapist) who conducts a clinical assessment of your mental health condition and determines therapeutic necessity. RealESALetter.com connects individuals with licensed therapists who perform compliant evaluations based on current clinical standards and legal requirements. The process includes mental health history review, symptom assessment, and determination of whether an ESA would ameliorate specific disability-related symptoms. For those specifically in Ohio, comprehensive ohio guidance is available.
What's the difference between an ESA and a service animal according to research?
Service animals receive extensive task-specific training to perform disability-related work (guiding blind individuals, alerting to seizures, etc.) and have broader public access rights under the Americans with Disabilities Act. ESAs provide therapeutic benefit through companionship and presence without specialized training, and protections cover housing and air travel only. Research shows both provide mental health benefits, but through different mechanisms—service animals through trained tasks, ESAs through the human-animal bond and routine care requirements. Those requiring trained psychiatric service dogs should explore PSD letter options for more extensive accommodations.
Are certain dog breeds better ESAs according to scientific evidence?
Current research doesn't support breed-specific ESA recommendations. Studies show that individual temperament, training, and human-animal bond quality matter more than breed for ESA effectiveness. The ideal ESA demonstrates calm demeanor, appropriate activity level for the owner's lifestyle, and strong bonding capacity. Claims about "best ESA breeds" lack scientific support—matching should focus on compatibility between individual animal temperament and owner needs.
How long does it take for ESA benefits to appear based on research?
Research indicates acute stress reduction occurs within 5-15 minutes of ESA interaction (measurable through cortisol and heart rate changes). Symptom improvement on clinical anxiety and depression scales becomes statistically significant at 6-12 weeks of consistent ESA accommodation. Maximal benefits typically emerge at 3-6 months as behavioral patterns stabilize and the human-animal bond strengthens. Long-term studies show sustained benefits lasting years when clinical monitoring continues.
Conclusion: Science-Informed ESA Accommodation
The scientific evidence overwhelmingly supports Emotional Support Animals as effective adjunct treatments for anxiety, depression, PTSD, and related mental health conditions when properly integrated into clinical care. Research demonstrates measurable neurobiological changes, clinically significant symptom reduction, and sustained long-term benefits for appropriately matched individuals.
The key to successful ESA accommodation lies in legitimate clinical evaluation by licensed mental health professionals who understand both the science and the legal framework. RealESALetter.com provides access to licensed therapists who conduct thorough, compliant assessments based on current research and clinical standards. Every evaluation examines diagnosed conditions, therapeutic necessity, and individual suitability for ESA care—ensuring accommodation requests rest on solid medical and scientific foundations.
The science is clear: when ESAs serve as therapeutic interventions under professional guidance, they provide real, measurable mental health benefits supported by peer-reviewed research. Understanding this scientific foundation protects both the legitimacy of ESA accommodations and the individuals who genuinely need them.














